The US Food and Drug Administration is officially taking action to remove phenylephrine, a popular decongesting ingredient, from medications taken orally, including some popular cold and flu over-the-counter drugs.
While phenylephrine is still considered safe, a scientific panel that advises the FDA found last year that it doesn’t actually work at decongesting or “unstuffing” your nose when it’s taken by mouth in over-the-counter products. Phenylephrine is still considered effective in nasal spray form.
Importantly, the FDA’s notice from this week doesn’t affect the sale of any medication right now; the FDA is seeking public comment on its proposed rule. If, after more consideration, the health agency decides to change the rules around phenylephrine oral over-the-counter products, it will be removed as an active ingredient and drugmakers will need to change their product formulas or pull them altogether.
“Based on our review of available data, and consistent with the advice of the advisory committee, we are taking this next step in the process to propose removing oral phenylephrine because it is not effective as a nasal decongestant,” Dr. Patrizia Cavazzoni, director of the FDA’s Center for Drug Evaluation and Research, said in a news release.
Oral phenylephrine is included in many popular medications like some NyQuil, Mucinex and more name- and store-brand kinds of oral medications, though some of them contain other ingredients besides phenylephrine that may ease symptoms. Ahead of official agency action, CVS last year pulled a “small number” of medications that contain phenylephrine as the only active ingredient (think Sudafed PE). The company said it “will continue offering many other oral cough and cold products to meet consumer needs.”
Many people use over-the-counter decongestants for milder symptoms of a virus or to treat their seasonal allergies. This makes them an easy first-line treatment. And according to Dr. Geoffrey Rutledge, chief medical officer and co-founder of the telemedicine site HealthTap, having choices when you’re feeling miserable can be one of the most important parts of treatment.
But you don’t have to settle for one option.
“As a physician in practice, I have never recommended patients use phenylephrine products,” Rutledge told CNET in 2023, after news around the FDA committee’s findings first broke. Instead, he directs them behind the counter for a more effective decongestant, pseudoephedrine, or to other medications if the source of congestion is allergies.
Medications that contain phenylephrine often contain other active ingredients, don’t throw away your meds just yet. Here’s what you should know about finding a decongestant heading into cold, flu and virus season.
What is phenylephrine?
Phenylephrine is a decongestant that works by restricting the blood vessels in your nose. It’s found in common medications like Sudafed PE (not regular Sudafed), Theraflu, Tylenol Sinus, Advil Congestion, NyQuil Severe Cold and Flu products and more. These are medications that don’t require a prescription, are easily available on store shelves and are typically meant to treat other cold or flu symptoms in addition to congestion.
Phenylephrine’s more effective cousin: pseudoephedrine
There’s another oral decongestant that works similarly, pseudoephedrine, and research has shown for a while that it’s more effective than phenylephrine, according to Dr. Stacia Woodcock, a pharmacist and pharmacy editor at GoodRx.
“The idea that phenylephrine doesn’t work isn’t a new one for most health care professionals,” Woodcock said in an email last year. “Pseudoephedrine (Sudafed) has clearly been the superior decongestant for quite some time.”
Pseudoephedrine, however, faces more restrictions because it’s also a main ingredient used to make methamphetamine. This means that while phenylephrine-containing Sudafed PE is available on store shelves, you probably have to ask a pharmacist and show ID to purchase regular Sudafed, which contains pseudoephedrine. There are also limits on how much you can buy at once. (Other names for pseudoephedrine medication include 12 Hour Cold Maximum Strength.)
As a result of the restrictions on pseudoephedrine, “most cough and cold medication manufacturers turned to phenylephrine to replace pseudoephedrine in their OTC products,” Woodcock said. “This allowed people to purchase them when the pharmacy is closed, if they’d reached their monthly limit on pseudoephedrine products, or if they didn’t have the necessary ID to purchase it.”
While pseudoephedrine is considered safe for most adults when taken as directed, it also works by constricting blood vessels and acts more like a stimulant. This means it’s a good idea to talk to your doctor before taking a decongestant (especially pseudoephedrine) if you have certain health conditions like high blood pressure, a heart problem, glaucoma, diabetes or if you’re pregnant or breastfeeding. A certain type of antidepressant, monoamine oxidase inhibitors (MAOIs), may also interact with pseudoephedrine and phenylephrine.
Read more: What to Know About the New COVID Vaccines This Fall
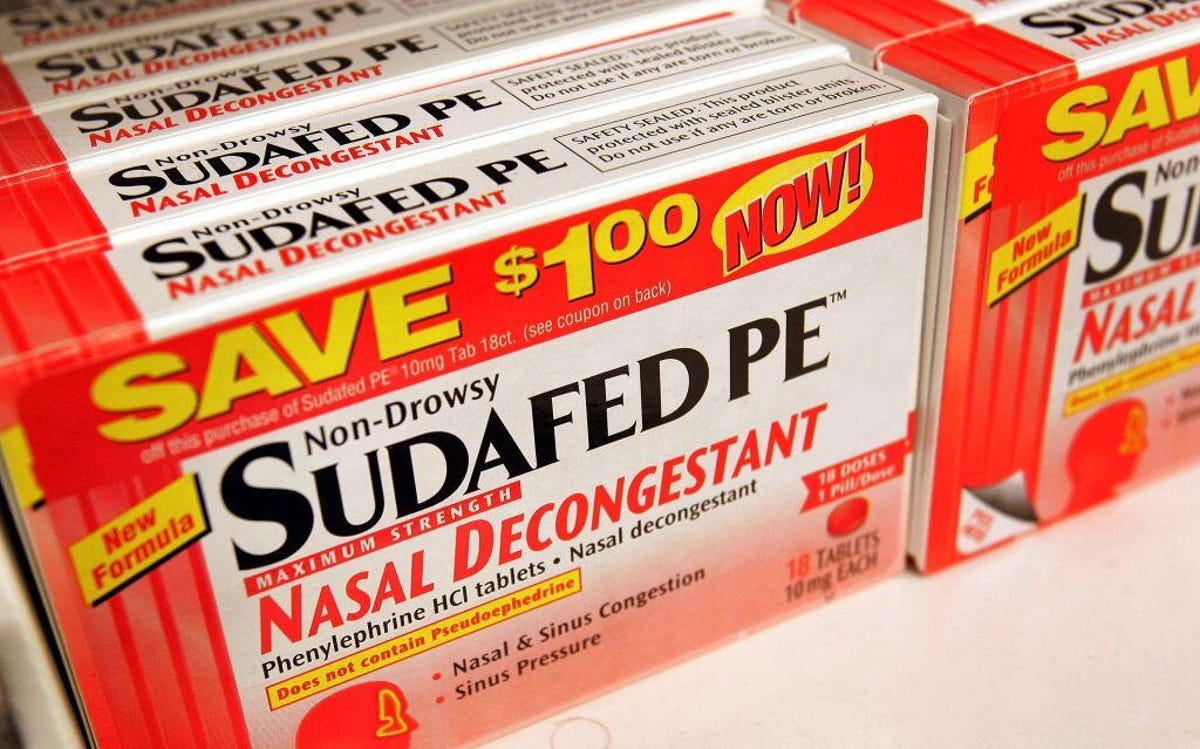
Sudafed PE is the phenylephrine-containing medicine you can pick up without talking to a pharmacist. (The “PE” stands for phenylephrine.) Regular Sudafed contains pseudoephedrine, and it’s what you want if you’re looking for a decongestant that works, according to Rutledge. You’ll have to ask a pharmacist for it, though.
Sudafed is just one of many brand names of medication that contain phenylephrine.
Don’t toss your meds yet
Oral decongestants containing phenylephrine have been on the market for decades. And according to survey information compiled for the FDA meeting by the Consumer Healthcare Products Association, many people are happy with products containing phenylephrine and say they’ve found a benefit.
According to both Woodcock and Rutledge, it’s fine to keep using products containing phenylephrine if you want to or you find they help. You’re still probably getting the benefits from the other ingredients in the medication. Nyquil contains phenylephrine for decongestion, but it also contains ingredients to reduce fever and pain and suppress cough, which may still provide relief and ease your symptoms during the worst days of your illness. The same is true for other medications with phenylephrine.
Beyond the effectiveness of other ingredients, we shouldn’t overlook the fact that someone expecting relief from their medication is more likely to get it, says Rutledge. He referred to this dynamic-duo effect on phenylephrine as “the power of placebo and the power of the other ingredients.”
The FDA committee considered evidence that suggested phenylephrine itself is no better than a placebo, or “dummy” medication used to test the effectiveness of something. But there are different angles to the placebo effect, Rutledge says.
“It’s been shown time and time again if you believe something will work, there will be a subjective measurable benefit,” he noted, adding that patient outcomes and treatment follow-throughs are better when patients believe in what their doctors are telling them.
Read more: Here’s Where You Can Still Find Free COVID Testing
Alternatives to oral decongestants
Nasal sprays containing phenylephrine are still considered effective decongestants, Woodcock said, because it goes right to the source of congestion and is better-absorbed by the body. They may also contain oxymetazoline. But nasal sprays come with a “big caveat,” she said. You can only use the spray for a few days or risk “rebound congestion” that’s difficult to get rid of and can last up to a year.
And if you want an oral decongestant that works, Rutledge said, ask for the pseudoephedrine. Common side effects can include shakiness or restlessness.
For congestion caused by allergies, you’ll need to target your symptoms a little differently, Rutledge says. A nasal-inhaled steroid like Flonase is better for long-term use by allergy sufferers because “rather than treating the symptoms, the steroid actually blocks the immune reaction in the nose,” he said.
Antihistamines are also used by people with allergies, but know that antihistamines aren’t decongestants, Rutledge said. They work by blocking the effect of histamine, which your body releases in response to an allergy. This is why one simple test for helping you figure out whether you have allergies or a virus is by seeing if your symptoms improve when you take an antihistamine.




















+ There are no comments
Add yours